Knee replacement surgery: for your information
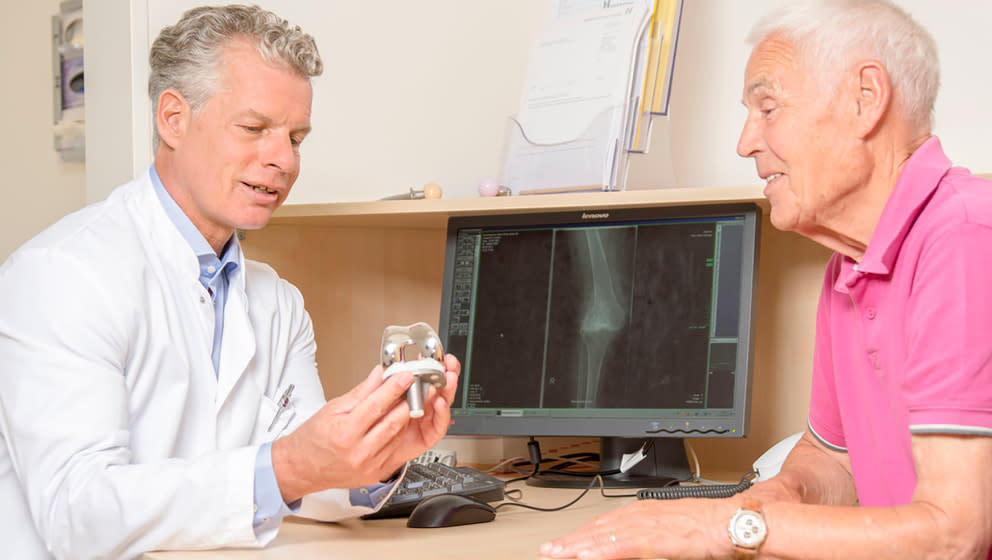
The surgeon chooses the correct surgical method according to the form and severity of the joint damage. Depending on how badly the knee is damaged, it may have to be partially or completely replaced.
The new knee joint
If the joint damage is too heavy and the physiotherapy no longer helps, the knee can be replaced in whole or in part by an artificial joint.
Structure of knee joint
When we walk, stand up, climb or go down the stairs, we use one important joint: the knee. Learn more about how it is organized.
Сauses of knee pain
Find out why your knees are starting to hurt.
Preparing for your hospital stay
Possible preliminary examinations and preparation for hospitalization
Preparation exercises before the surgery
Find out which exercises will help you recover more quickly from surgery, rehabilitate more effectively, and improve your chances of achieving your health goals.
How is hospital treatment going
What does the hospital expect? Learn in advance how everything is organized.
After the orthopaedic surgery
Postoperative period and recovery
Being able to smile again: the Olympic Games as a goal
Katsiaryna Halkina is 23 years old, and has been active in sports since she was five years old.
As well as for many professional athletes, the Covid-19 pandemic has disrupted Katsiaryna’s plans to attend the Tokyo Olympics 2020, which have been postponed to 2021. However, besides the COVID-19 pandemic, she suddenly has started feeling pain in her right foot.
Patient story: innovative joint surgery brings new hope to a dancer
For five years, the girl had unsuccessfully tried various treatment methods until she underwent an innovative procedure that is currently offered only at the Helios Hospital Krefeld, Germany. Thanks to this procedure, she has already started training and is preparing for her return.
Customized knee joint prosthesis
Artificial knee joint should fit the bone like a tailor-made suit because each knee joint is unique.
Patient Story: Congenital deformity of the spine involving lateral curvature (scoliosis)
The 16-year-old hid her crooked back under large T-shirts and wore a painful corset. But her spine continued to curve. Only surgery could help her – and it also increased the girl's height by five centimeters.
Ortho Fast Track recovery
With the accelerated recovery method, patients get up on their feet on the day of surgery, experience less pain, and spend less time in the hospital.
Robot-Assisted Knee Joint Surgery Using Rosa Robot
A new computerised robot-assisted system is now used in knee joint surgical interventions by the orthopedic team at Helios Hospital Berlin-Buch. It optimizes the knee joint prosthesis adaptation and ensures its optimal fit. It ensures increased patient satisfaction with an artificial joint.
Every day, 6 to 10 arthroplasties are done in an operating room at Helios Krefeld
Today we are talking to Prof. Dr. Med. Clayton Kraft, head of the clinic for orthopedics, trauma, and hand surgery at Helios Hospital Krefeld, about orthopedic procedures as well as modern and traditional approaches in endoprosthetic surgery.
Branch of the renowned ENDO-Klinik Hamburg opens at Helios Hospital Berlin-Buch
As of June 1, Helios Hospital Berlin-Buch will be a partner hospital of Europe's largest specialist clinic for endoprosthetics, sports orthopedics and spine surgery - ENDO-Klinik Hamburg. After two years of preparation, endoprosthetic care at the highest medical level is now available to all patients in the region.
New robotic technology for knee joint replacement at Helios Hospital München West
DIGITALIZATION IN ENDOPROSTHETICS
Patients who receive an artificial knee joint at the Helios Klinikum in Pasing will in future benefit from human expertise and the latest technology.
First robotic surgery at Helios Hospital München West
At the Endoprosthetics Center Munich West, a knee prosthesis has been implanted for the first time using robotic arm-assisted technology. The new Mako system offers more safety and precision for patients.
The "Ortho-Campus" in Hüls: A modern treatment concept for hip and knee replacement surgeries
“All-in-one”: The "Ortho-Campus" in Hüls as part of Helios Hospital Krefeld offers joint replacement and rehabilitation under one roof. There is no need anymore to switch between the hospital, where the surgery is carried out, and a rehabilitation center. The same surgeon and medical team accompany the patient throughout his/her whole process: from the first consultation and taking the decision for surgery, during the surgery and even into rehabilitation.
The "bikini" incision: less pain, less blood loss and faster recovery in hip surgeries
Assoc. Prof. Dr. Martin Thaler, head of endoprosthetics at Helios Hospital München West, is a pioneer of a particularly gentle surgical technique for hip operations. He has been operating on patients for over 20 years using the so-called bikini incision.
Helios Cäcilien-Hospital Krefeld-Hüls: Patient Testimonials Ortho-Campus
Real patients report - people of different ages tell their stories: About their joint pain and surgery, rehab and how it is to live with the new knee or hip joint.
Helios Hospital Siegburg: Artificial hip joint - gentle surgery and fast mobilization
When is an artificial hip joint used? How does the operation proceed? And how do patients who are operated on at the Helios Klinikum Siegburg benefit? We asked Dr. Dennis Vogel, head physician for special orthopedic surgery, endoprosthetics and foot surgery.
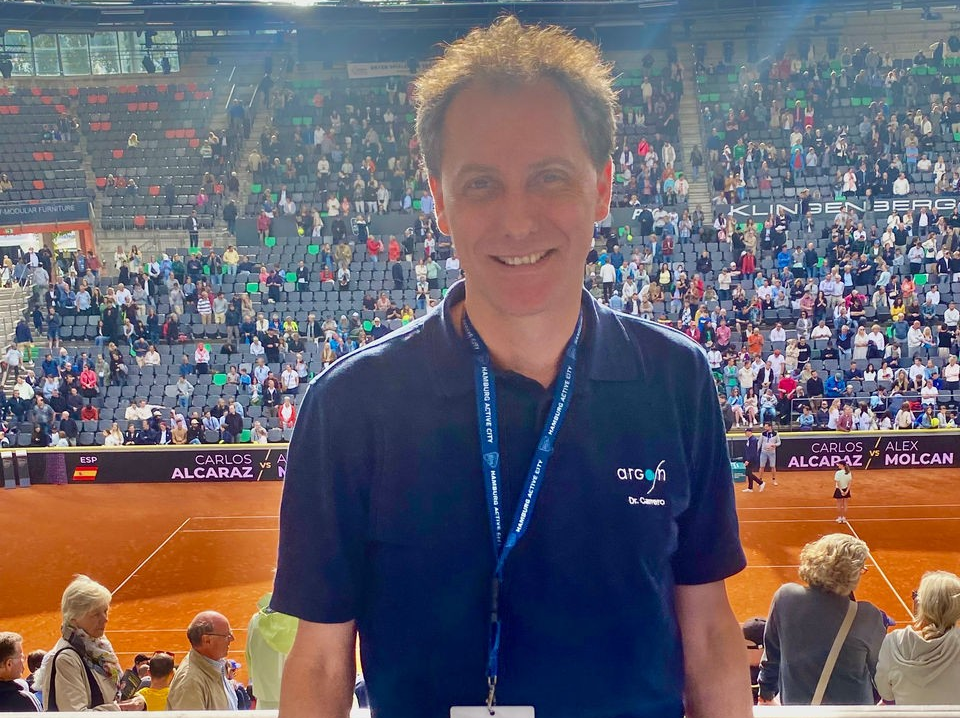
World-class tennis with experts from ENDO Clinic and ENDO Rehab Center
The Hamburg Open will continue to rely on the ENDO-Clinic Hamburg, the ENDO Rehab Center and the MVZ arGon as its sports medicine partners in 2024. The team is led by Hamburg orthopedic surgeon Dr. Volker Carrero, who is entering his sixteenth year as tournament doctor at Hamburg's Rothenbaum.
Helios Hospital Siegburg: Joint embolization - new therapy for painful knee prostheses
Pain relief through special sclerotherapy of the vessels
According to statistics, around 200,000 people in Germany receive an artificial knee joint (total knee arthroplasty, knee TEP) every year. One of the main reasons for the use of such a prosthesis is cartilage wear (osteoarthritis) in the knee, less frequently inflammation or injury. As a rule, the use of a knee TEP leads to significant pain relief, greater mobility and therefore also to a better quality of life. "In rare cases, however, patients continue to struggle with chronic pain without us being able to find a tangible cause. We now know that chronic inflammation of pathological, newly formed vessels around the knee can be one of the causes of the pain," explains Dr. Dennis Vogel, Head of Special Orthopaedic Surgery, Endoprosthetics and Foot Surgery at Helios Hospital Siegburg.
Helios St. Elisabeth Hospital Oberhausen: Back on your feet after bilateral hip surgery
Daniela Wehrmann had an artificial hip joint (hip TEP) fitted on both sides in just one operation - and she was already taking her first steps the day after the procedure.