Сauses of knee pain
Why do my knees start to hurt?
The most common cause of knee pain or other complaints about knee joints is age-related destruction of joint cartilage. These changes are also called knee joint osteoarthroses or, in a different way, gonarthroses. Typical symptoms are swelling and redness in the knee area, increased muscle tension, unusual sounds ("friction noises") or deterioration of stability and volume of movement.
Such pathological changes are a natural process of aging and can develop without any visible cause.
The knee joint consists of three bones: the tibia, the femur and the patella. The joint surfaces of these bones are covered with a soft cartilage layer, which softens the shocks and prevents the bones from friction against each other. But for various reasons, the knee may be subjected to increased stress and damage, which eventually leads to the destruction of the protective cartilage layer. In such cases, painful sensations develop.
Since people suffering from pain in the knees, trying to do as little painful movements as possible and forced to take gentle poses, the problem with the knees is even more intensified. The lack of movement leads to an almost literal drying of the cartilage, which means that its protective ability is becoming more and more impaired.
Types of knee arthrosis
The development of knee joint osteoarthritis may be caused by deformities of the lower limbs, prolonged excessive loads or incorrect load distribution, rheumatic diseases, metabolic diseases or injuries. All this leads to the appearance of cracks in the protective layer of cartilage of joint surfaces: cartilage begins to break down. The knee joint is gradually covered by inflammation, and it begins to deform. In everyday exercise, such as prolonged walking, painful sensations occur, and the further the disease has gone, the shorter the path that can be overcome without pain. In addition, the joint develops more and more stiffness.
Such pathological changes are possible not only in old age. Sometimes gonarthrosis develops even before the age of 30, for many reasons. In some cases, an unambiguous cause cannot be identified, which tells us about primary or idiopathic arthrosis. If there are external causes, secondary arthrosis develops. Among the varieties of secondary arthrosis is, for example, post-traumatic arthrosis - pathological changes in the joint caused by trauma to the bones or cartilage, which may develop even a few decades after the trauma.
1. Primary (idiopathic) arthrosis
In case of primary or idiopathic osteoarthritis it is not possible to determine the unequivocal causes of its development. Doctors call it "obscure etiology". Although it is still unclear how and why primary arthrosis begins to develop, scientists believe that the appropriate tendency is inherited. However, the propensity to develop osteoarthritis, even if it is observed in the family, is not yet.
2. Secondary osteoarthritis
In secondary arthrosis, doctors are able to determine which disease or injury led to its development. Risk factors include rheumatism, excess weight, metabolic problems with local circulation or deformities of the lower limbs.
Widespread, for example, deformities such as valgus (where the legs take the form of the letter X) or varus (where the legs take the form of the letter O). As a car wheel, which is broken "camber-like" knee joint is subjected to increased one-sided loads: with a valgus deformation - on the outside, with a varus - on the inside. This leads to premature destruction of articular cartilage. Such deformations are often congenital, but may also develop if the broken bones do not join together correctly.
¹ The name of several different diseases, often caused by inflammation and affecting, for example, the joints, vertebrae, cartilage and nerves. Rheumatoid arthritis - chronic inflammation of the joints.
3. Post-traumatic arthritis
Osteoarthritis may also develop after an injury, then it is called post-traumatic. The cause of such osteoarthritis is damage to the joint surface, meniscus or ligament system. The occurrence of post-traumatic osteoarthritis may also occur many years after the injury.
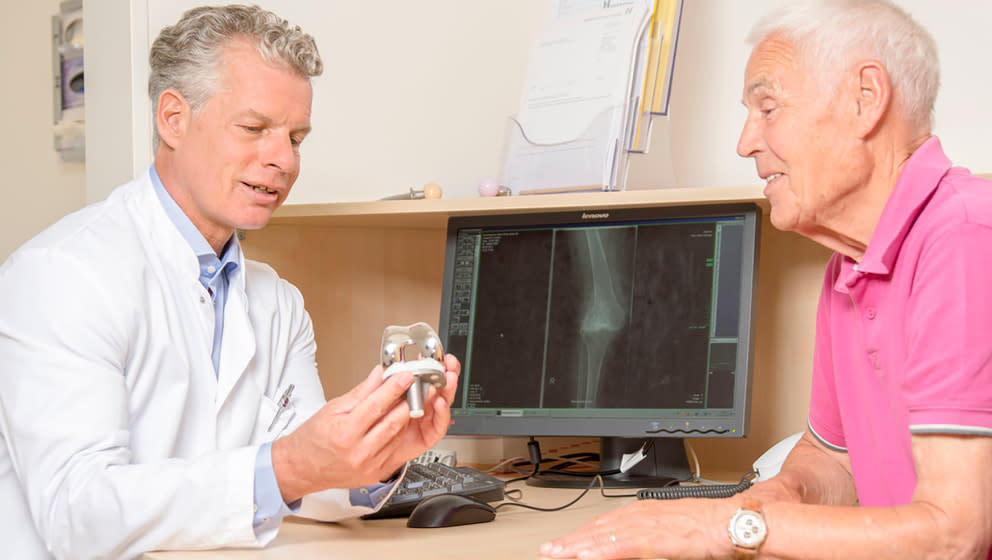
Unfortunately, there is no cure for osteoarthritis completely. But in the initial stages of the disease complaints may decrease after classical therapies, such as physiotherapy (previously - therapeutic physical training, prescribed by a doctor) and electrotherapy (therapeutic use of current flow, for example, to reduce pain).
But if the disease is neglected, doctors have to resort to prosthetics of the knee joint. Of course, we know that no artificial joint can compare to a person's own joint, so we, if possible, seek to conduct joint-preserving surgery. Our goal is to preserve patients' own joints for as long as possible.